Abstract
Background: Allogeneic hematopoietic stem cell transplantation (HCT) is a curative therapy for many hematologic and non-hematologic diseases; however, it is associated with significant morbidity and mortality. Many studies have shown that elevated pre-transplant ferritin levels are associated with increased risk of morbidity and mortality following HCT. Given ferritin's association with systemic inflammation, it is a plausible potential prognostic marker in the post-HCT period, including in patients with graft-versus-host disease (GVHD). The present study attempts to determine whether post-transplant serum ferritin level is an independent prognostic marker for outcomes post-HCT, especially in the subgroups of patients with acute or chronic GVHD.
Methods and patients: A total of 229 patients who had serum ferritin level data available within one-year post HCT were enrolled into this retrospective study. These patients underwent HCT at Princess Margaret Cancer Centre, Toronto, Canada between 2001-2013. Patients' characteristics and transplant procedures were: median age: 51 (range:19-70); refined disease risk index: low (n=70), intermediate (n=108), high (n=51); donor type: HLA-matched related donors (n=94), HLA-matched or partially-matched unrelated donors (n=135); conditioning regimen: myeloablative (n=120), reduced intensity (n=109).
Acute and chronic GVHD were respectively classified using the 1994 consensus conference and NIH consensus criteria. Primary outcomes were overall survival (OS), non-relapse mortality (NRM), and relapse. Kaplan-Meier method was used for OS; cumulative incidences were used for NRM and relapse, considering competing risks. Multivariate analysis employed Cox or Fine-Gray proportional hazard regression model. Factors evaluated included recipient age and CMV status, donor-recipient sex, comorbidity score, performance index, GVHD prophylaxis, post-transplant serum ferritin level (ferritinPost-HCT), and serum ferritin level prior to HCT (ferritinPre-HCT). Recursive partitioning was used to stratify patients into low or high risk groups based on ferritinPost-HCT (≤3,169 vs >3,169 ng/mL) and ferritinPre-HCT (≤669 vs >669 ng/mL).
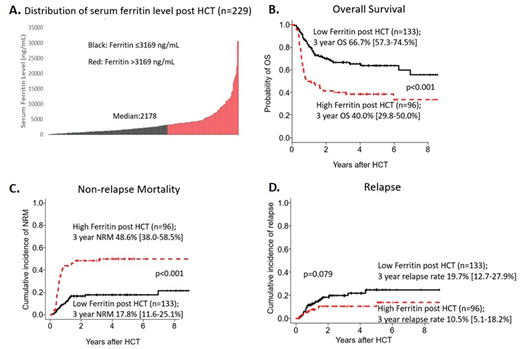
Results: Median follow-up duration among survivors was 46 months post-HCT (range:2.8-147.2 months). Median ferritinPost-HCT was 2,178 ng/mL (range: 45-30,647; Figure A), measured at a median of 137 days post-HCT. There was a weak correlation between ferritinPost-HCT and ferritinPre-HCT (Pearson's correlation r=0.242, p=0.002).
Compared to the group with low ferritinPost-HCT, the high ferritinPost-HCT group had lower three-year OS (40.0% vs 66.7%, p<0.001; Figure B) and higher NRM (48.6% vs 17.8%, p<0.001 Figure C), but no difference in cumulative incidence of relapse (10.5% vs 19.7%, p=0.079; Figure D). A landmark analysis was performed where the day of ferritinpost-HCT measurement was considered day 0. Results of this landmark analysis showed consistent findings: high ferritinPost-HCT showed lower three-year OS (38.3% vs 65.4%; p<0.001) and higher NRM (50.6% vs 17.7%; p<0.001) compared to low ferritinPost-HCT, but no difference in relapse (10.7% vs 21.3%, p=0.077). In multivariate analysis, ferritinPost-HCT was found to be an independent prognostic factor for OS (p=0.001, HR 2.323) and NRM (p<0.001, HR 3.905). However, pre-transplant ferritin level (ferritinPre-HCT) did not stratify well for OS (57.0% vs 61.8%, p=0.636) or NRM (30.8% vs 22.7%, p=0.247).
Out of 229 patients, 171 (74.6%) developed any grade of acute GVHD, and 61 (26.6%) developed chronic GVHD. Median onset of acute and chronic GVHD were, respectively, 33.5 days and 145 days. Level of ferritinPost-HCT was significantly higher in the group that developed acute GVHD than in those without acute GVHD. However, there was no difference in ferritinPost-HCT between patients with or without chronic GVHD. FerritinPost-HCT was found to be an independent prognostic marker in the subgroup with acute GVHD for OS (p=0.001, HR 2.531) and NRM (p<0.001, HR 3.584), and in the subgroup with chronic GVHD for OS (p=0.042, HR 3.226) and NRM (p=0.009, HR 14.130).
Conclusions: In our cohort, high ferritinPost-HCT levels were significantly associated with decreased OS and increased NRM, independent of other prognostic factors including ferritinPre-HCT or GVHD. Further prospective study including larger number of patients is warranted.
Lipton:ARIAD: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding. Kim:BMS: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy; Novartis: Consultancy, Honoraria, Research Funding; Paladin: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal